The buzz on Utah’s fledgling medical cannabis program – Leafly
Ashley SchwellenbachFebruary 19, 2020
Share
Print

(Legacy Images/AdobeStock)
The state of Utah is famously conservative, both politically and culturally. In a region of the country dominated by liberalism, Utah’s elected officials are overwhelmingly Republican. The state hasn’t had a Democratic governor in 35 years and hasn’t voted for a Democrat in a presidential election since 1964. Life in the Beehive State is largely dictated by the powerful Mormon church, which has historically vocally opposed marijuana legalization.
So when the state’s voters passed Proposition 2, the Utah Medical Cannabis Act, it wouldn’t have been a surprise to see legislators undermine voter intentions with a painfully slow rollout or outright disregard. Instead, to the surprise of many, Utah legislators and regulators have wasted no time developing a thoughtful, functional medical marijuana system that actually serves its patients.
How did that happen?
Voters led, and leaders followed

Republican Sen. Mark Madsen of Eagle Mountain speaks on the latest of two competing plans to allow people with certain medical conditions to use marijuana at the Utah State Capitol Friday, Feb. 19, 2016, in Salt Lake City. (Rick Bowmer/AP)
It’s been more than two years since Utah voters surprised the nation by passing Proposition 2, the Utah Medical Cannabis Act. Utah became the thirty-third state to legalize medical cannabis, not altogether significant for broader legalization efforts, but a giant step for the Beehive State, which is considered to have one of America’s most conservative populations.
Less than one month later, the Utah Legislature passed HB3001, controversially amending the voter-approved initiative and instituting a March 1, 2020, deadline for the Utah Medical Cannabis Program to issue patient registration cards, register medical providers qualified to approve patients, and license medical cannabis pharmacies.
In the meantime, patients with qualifying conditions can procure a letter of recommendation from their doctor, drive to neighboring Colorado or Nevada to make their cannabis purchase, and return to Utah to consume it without the threat of prosecution. It’s an imperfect system. But stakeholders generally agree the state’s bureaucracy is rolling out the program at record pace by legislative standards. More importantly, they’re trying to get it right.
Defining getting it right

Richard Oborn, director of the health department’s Center for Medical Cannabis speaks during a hearing Wednesday, Jan. 29, 2020, at the Utah State Capitol, in Salt Lake City. (AP Photo/Rick Bowmer)
Getting it right starts with hiring the right people—like Richard Oborn. In October 2018, the state hired Oborn, formerly employed with the Utah Department of Finance, to direct Utah Department of Health’s Center for Medical Cannabis. Proposition 2 hadn’t even passed yet, but it seemed inevitable and legislators didn’t want to waste any time. A year earlier a poll conducted by the Salt Lake Tribune-Hinckley Institute of Politics revealed that 77% of Utah voters supported legalizing medical cannabis.
It was Oborn’s first experience creating a statewide medical cannabis program, but he had an advantage his counterparts in earlier states did not: prototypes. “One thing that’s important for us is to learn from experiences in other states,” Oborn told Leafly in a recent interview. “We’ve been doing a lot of research about what’s worked in other states and what hasn’t.”
Oborn cites Minnesota as a state that has done a good job polling patients for data that can improve the program and educate the public, for example. That’s something he’d like to see Utah incorporate.
He’s also looked to other states for ideas about how to handle limits on advertising. Oborn’s team studied programs that require state approval of all educational materials available at dispensaries—or “pharmacies” as Utah’s Center for Medical Cannabis refers to them. Ultimately, Oborn and his department decided not to expend limited resources vetting every last piece of literature.
Another major challenge in Utah is accessibility. It’s a small-population state with a large land mass. Economies of scale may be hard to come by for dispensaries. “How do we keep the price reasonable for patients?” said Oborn. “The cost is a concern for patients. It’s a concern for us. Federal restrictions make it so insurance can’t help cover the cost. It has to be 100 percent grown, processed, and sold in Utah and that’s a challenge to the cost.”
Unfortunately, there are some answers that not even the early adoption states can provide. Utah’s hunt for substantive medical marijuana research, for example, was stymied by the U.S. government’s longstanding war on drugs, which prevented most research into the medical effects of cannabis. The state instead turned to studies conducted in Canada and Israel to provide the necessary data to help guide their program.
Oborn hopes the federal government will reform its stance on marijuana in the near future to enable more research and offer a solution to the lack of banking services available to state-legal companies. Absent full-scale federal legalization, Oborn is just trying to create the best program he can in the face of all the limitations, challenges, and unknowns.
A “normal” retail experience
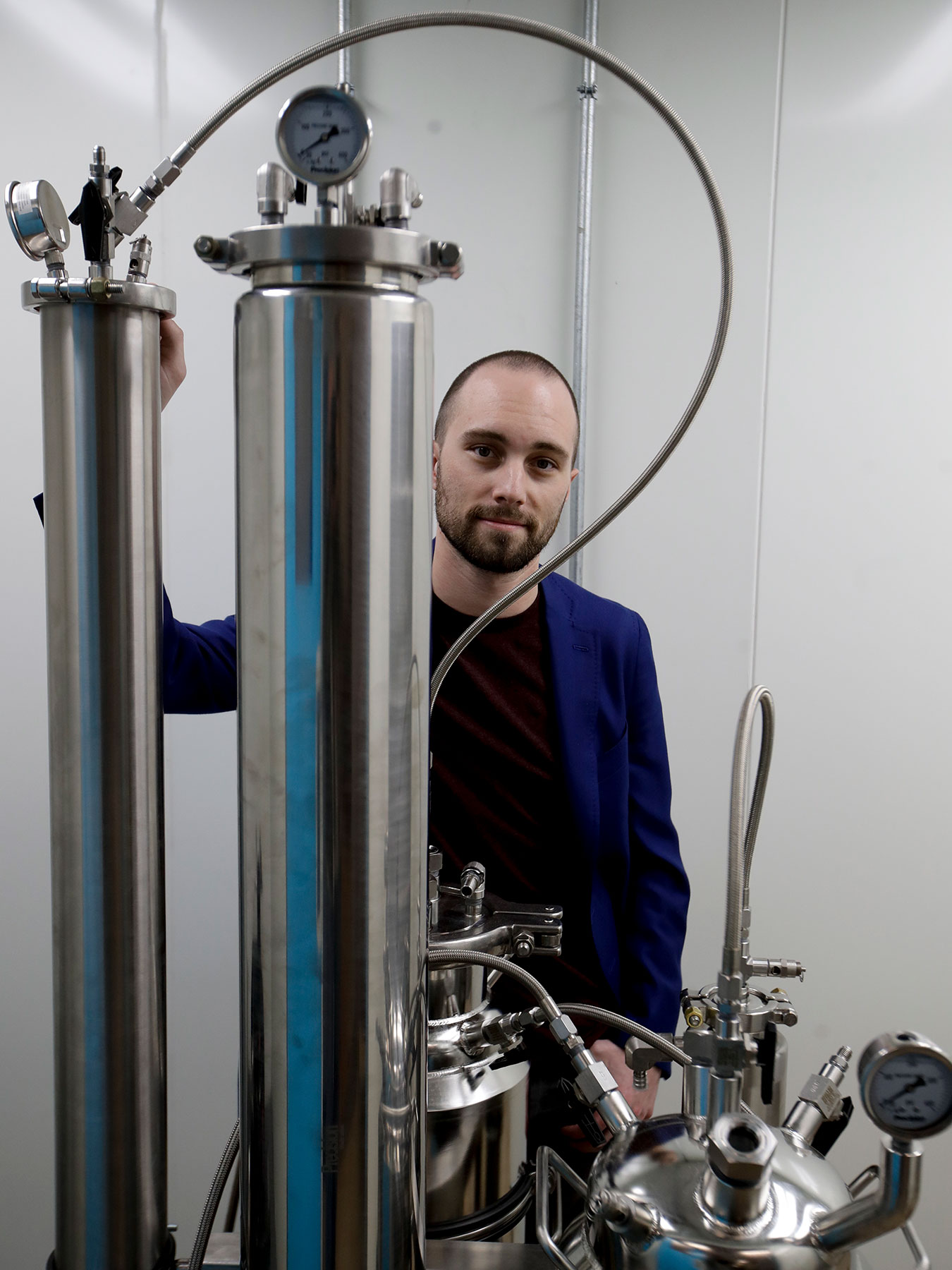
Jordan Lams, CEO of Moxie, poses for a picture next to a precision extractor Thursday, Dec. 14, 2017, in Lynwood, Calif. (AP Photo/Chris Carlson)
On January 3, the Utah Department of Health announced it would issue 14 medical cannabis pharmacy licenses to 10 different companies, four of which would receive licenses to open two stores. Pure UT, a wholly owned subsidiary of Moxie, was one of the companies awarded a single license. (Moxie is a California-based cannabis brand with subsidiaries in Nevada, Michigan, and Pennsylvania.) Pure UT currently plans to open a medical cannabis pharmacy in the northeastern Utah city of Vernal later this year.
As multi-state operators already active in four states, the Pure UT and Moxie team have been through this process several times over and have strong opinions about how states can set themselves—and their programs—up for success. Pure UT Principal Jordan Lams told Leafly he likes to get involved early, working with state officials to provide input into the developing regulatory framework.
So far, Lams has been impressed with Utah’s approach. “We’re excited by the agility with which the regulators and legislators have approached the iterative process of regulating,” Lams said. “You’re never going to get it all right out of the gate. What’s really going to drive the success of any new market is the ability of the legislators and the regulators to make changes quickly to ensure that they’re doing the best to balance business, patient access, affordability, and safety.”
Why choose Vernal?
Pure UT’s choice of location speaks to an unorthodox business plan and philosophy. The city of Vernal, with 9,000 residents, doesn’t even crack Utah’s top 50 cities by population. But the price of real estate is one of the most significant costs of operating a cannabis business. So there may be some advantage to entering the small-town market.
Utah is one of America’s least densely populated states, which could make it difficult for little more than a dozen medical cannabis dispensaries to service the needs of a widely scattered population.
Lams believes there’s a compelling reason to choose Vernal: If Pure UT didn’t open there, who would?
“Part of our investment thesis as a company is to go to the areas where we could have a meaningful impact,” Lams said. “In assessing Vernal, we think it’s an area that serves a lot of people from a broad region. Also, we believe that what we do will be recognized and valued by the community. It’s a place where we can get ingrained. And that’s similar to what we do in every state.”
Doctors are hesitant

This Wednesday, Oct. 23, 2019 photo shows Medical marijuana advocate Christine Stenquist, at the Utah State Capitol, in Salt Lake City. (AP Photo/Rick Bowmer)
Just three months after the Utah Legislature passed HB3001 on December 3, 2018, Dr. Corey Anden began seeing medical cannabis patients in Ogden, Utah. Anden is quadruple board certified, specializing in sports medicine and non-surgical orthopedics. After 30 years of medical practice in Utah, she had no hesitation about participating in the state’s medical cannabis program.
Unfortunately, she’s the exception, not the rule.
A Fox 13 report in late 2019 found that prospective Utah patients struggled to find doctors willing to recommend cannabis. Some patients, including an 8-year-old girl in hospice, reported spending months visiting multiple doctors before they found one willing to prescribe medical marijuana. Some refuse because of decades of anti-cannabis rhetoric. Others want to prescribe medical cannabis but fear a backlash—including the possibility of losing their medical licenses.
As a result, doctors like Anden find themselves with a long waiting list of patients desperate to see them.
In the last year she’s provided medical cannabis referrals for nearly 600 patients from all corners of the state, some of whom travel upwards of five hours to see her.
Under the current system, which will change on March 1, Anden writes a letter of recommendation and the patient drives across the Utah border to legally purchase their cannabis in Colorado. (They could do that anyway, if they’re 21 or older, but the doctor’s letter keeps them legal once they’re back home in Utah.) After decades of witnessing the effects of patients being prescribed potent pharmaceuticals including opioids, the decision to offer her patients an alternative treatment was a no-brainer for Anden.
“What I’m doing now is legitimizing their use and explaining to them why it’s working,” Anden explained. “I do feel like I’m educating patients on how they could be using cannabis better. I spend a lot of time explaining how a vaporizer works. Many people also don’t realize there are ways of using cannabis without the intoxicating effects.”
The majority of Anden’s medical marijuana patients suffer from chronic pain, but she also treats PTSD, gastrointestinal issues, and children with autism. “I feel like I should be seeing more people with cancer but it looks like oncologists aren’t embracing the idea of cannabis,” she said with frustration.
The medical cannabis advocacy group TRUCE Utah points out that as long as there is a conflict between federal and state law on cannabis, many medical professionals feel they’re exposing themselves to risk by taking part in the state’s program. “The way our current Utah law is written puts doctors in direct harm’s way with the federal government,” TRUCE Utah president Christine Stenquist was quoted as saying in a separate Fox 13 article that ran February 11. “I have a physician on my board cautioning his colleagues not to enroll in the program.”
Utah’s medical provider shortage might not get any easier when the Utah Medical Cannabis Program officially goes online March 1. Participating doctors are limited to just 300 medical cannabis patients, a cap intended to prevent medical professionals from solely catering to cannabis patients.
Physicians will have the option of petitioning the Compassionate Use Board to increase the number of patients by up to 100 a total of three times, putting the absolute maximum at 600 patients.
Anden is frustrated by the limitation, pointing out that she could legally prescribe opioids to a potentially infinite number of patients. “I question the ethics and legality of that,” she said.
Richard Oborn didn’t have a hand in establishing patient limits, but the state health official acknowledges that it may be a problem.
“I think that is something we’ll wait and see on,” he told Leafly. “It’s possible there will be a small number of providers. It’s also possible that won’t be an issue.”
A paradigm shift

In this Jan. 28, 2019, file photo, the floor of the Utah House of Representatives is shown during the first day of the Utah legislative session, in Salt Lake City. Utah lawmakers are expected to meet Monday night, Sept. 16 to consider changes to the state’s medical marijuana law, an issue that has faced fierce criticism from people on both sides of the debate. The proposed changes include scrapping plans for an unusual state-run dispensary system and adopting protections for patients who are concerned they could be prosecuted for drug crimes. (AP Photo/Rick Bowmer, File)
Utah’s stakeholders represent diverse perspectives, but they all seem to agree the Beehive State’s medical cannabis program isn’t going to be perfect right out of the gate. Which is alright because they also share one auspicious quality: a commitment to getting it right.
Over the course of his time spent researching existing medical cannabis programs, Oborn never found a perfect model. “We haven’t identified any state where we’ve said ‘we want to do our program exactly like that one,’” Oborn said. “There’s no perfect program out there.”
But from Jordan Lams’ perspective, you don’t need a perfect program to improve people’s lives and health. What’s needed, said the Pure UT executive, is a paradigm shift. And that’s exactly what cannabis represents.
“Cannabis, from a medical standpoint, is a major shift in the way we approach self-care and the process of self-discovery,” he said. “Figuring out what works for you and your individualized health is a huge component of the healing process. We are all so unique. Our body chemistry is reflective of that. It’s not just in our personalities, our backgrounds, or our hair color, it’s in the way that our bodies react to the environment and the things that we put into our bodies so why in the world should we continue down this path of ‘you have this, you get the same thing as everyone else.’”
“Why does taking care of yourself have to have this automatic association with discomfort and pain?” Lams added. “If you ever see someone going through cancer treatment it’s one of the most miserable things you can ever watch someone you love go through. Why isn’t it possible that there’s an alternative that could be safe and natural and maybe even enjoyable to partake? Life should be enjoyed, including the part of taking care of yourself. Preventive or not, it shouldn’t have to suck.”
Share
Print

Ashley Schwellenbach
Leafly News Editor Ashley Schwellenbach is the former managing editor of the San Luis Obispo New Times and the author of Scourge of the Righteous Haddock, Vestal, and The Wheel Diver.
Related articles
Let’s block ads! (Why?)


